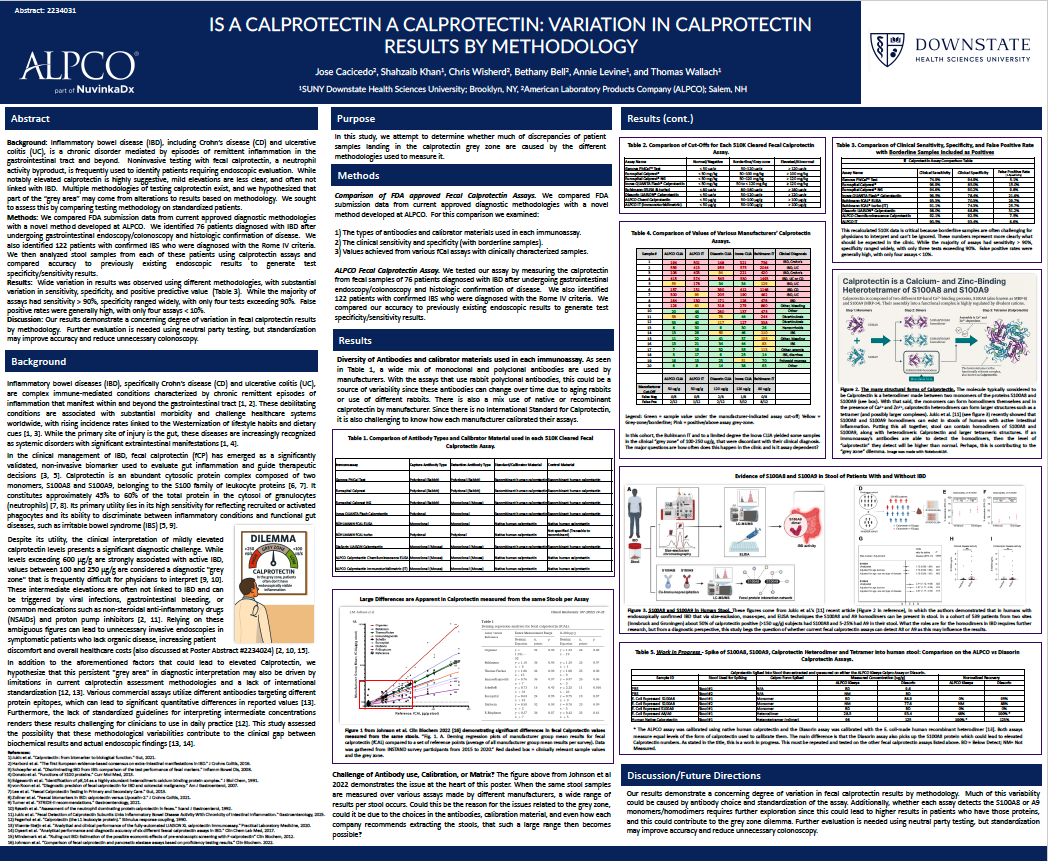
Fecal calprotectin (fCP) is a widely used, non-invasive biomarker to help distinguish inflammatory bowel disease (IBD) from functional conditions like IBS. But what happens when the same stool sample produces different results depending on the assay used?
New research suggests that differences in testing methodology — including antibody choice, calibration materials, and what forms of calprotectin are detected — may be contributing to the persistent clinical “grey zone” (100–250 µg/g).
In a head-to-head comparison of FDA-cleared assays and a novel ALPCO method, investigators observed wide variability in specificity and false-positive rates across platforms, raising important questions about standardization and clinical interpretation.
Want the full data? Download the complete poster abstract to explore the findings in detail.